| |
WHO, WHAT & WHY LIVES IN YOUR DIGESTIVE SYSTEM TO GIVE YOU LIFE EMPOWERMENT......
Posted by Vishva News Reporter on August 5, 2007 |

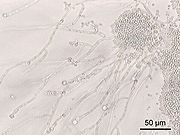
When a person is healthy, the gut flora is “in balance”
as shown in the stomach photo above. All 1000 different bacteria species go
along very well in the human digestive tract.
WHAT LIFE LIVES IN YOUR GUT AND WHY? AND WHERE
IT COMES FROM?
The Creator creates a pure human body at birth and then makes
it co-exists with all the rest micro-organism creations that the Creator creates
for the total well-being of a human. Proof as this statement is in the following
information on what exists in your stomach and the 32 ft of tube that connects
the stomach to your anus:
- The gut flora are the
microorganisms that normally live in the
digestive tract and can perform a number of useful
functions for their hosts.
- The average human body, consisting of
about 10 trillion (1013)
cells,
has about ten times that number of microorganisms in the
human gut, meaning about 100 trillion bacteria.
-
Bacteria make up most of the flora in the
colon]
and 60% of the mass of
feces.
- Somewhere between 300
and 1000 different
species live in the gut,
with most estimates at about 500.[
- However, it is probable that 99% of the bacteria come from
about 30 or 40 species.
- Fungi also make up a part of the gut flora, but little
is known about their activities.
- Research suggests that the relationship
between gut
flora and humans is not merely
commensal (a non-harmful coexistence), but rather is a
mutualistic,
symbiotic relationship.[
- Though people can survive with no gut
flora,
the microorganisms perform a host of useful functions, such
as
fermenting unused energy substrates, training the
immune system, preventing growth of harmful species,
regulating the development of the gut, producing vitamins
for the host (such as
biotin and
vitamin K), and producing hormones to direct the host to
store fats. However, in certain conditions, some species are
thought to be capable of causing
disease by causing
infection or increasing
cancer risk for the host.
Development of the gut flora
(photos and write from
www.probiotic-amsterdam.org/forlife/flora.htm)
A human being is being developed in the sterile environment of the uterus and at
birth it comes in touch with bacteria for the first time. This is the first step
in the colonization of the gastrointestinal tract of the newborn2. After birth
the newborns are exposed to numerous environmental agents (antigens),
particularly through food3. The intestines are important in the protection of
the human body against potentially harmful agents in food. This protection is
partly mechanical, but the fact that the intestinal mucosa forms an
immunological barrier is also important2. This mucosa represents a first line in
host defence.
The microbes in the intestines are important in the
development of the immune system. But they also help in degrading the food, in
detoxification of the intestines and are suppliers of essential vitamins4. The
microbial flora is relatively stable, once it has been established in infancy,
provided there are no major changes in the diet.
In ‘normally’ born children the colonization of the intestines
occurs during the first week of life. First the intestines are colonized with
facultative anaerobes, then with lactobacilli and bifidobacteria and finally
with bacteroides. In children that are born by caesarean, colonization of
intestines takes more time and does not show the same order of species. Early
colonization of intestines is needed for a good development of the immune
system2.
|

When the normal situation is disturbed, a so-called disbalance
arises or “dysbiosis” as shown in the human digestive tract photo above.
Functions of the gut flora
(photos and write from
www.probiotic-amsterdam.org/forlife/flora.htm)
Digestion is an important function of the gut flora. Many
nutrients from food that we eat are so large and complex that they must be split
into smaller parts before they can be used as energy. The process of breaking
down food into smaller parts is called digestion. Enzymes produced by bacteria
in the gut help breaking down the food. Other bacteria can produce vitamins B
and K.
The gut flora also has a protective role; the defence against
pathogenic organisms and other foreign components (allergens).
By adhering to the gut wall probiotics prevent pathogens to settle in the gut
and to multiply. In addition to this gut flora can produce several antimicrobial
components (acid, peroxide, bacteriocins) that mainly adverse the pathogens.
Besides this, toxins could be caught and carcinogenic or mutagenic substances
could be broken down.
(
Now current biological sciences is trying to figure out
where the micro-organisms in human digestive systems comes from when there
is none at birth time....following is the summation of this research:
- The current medical world knows our DNA from one end to the other, but can’t say the
same about the intestine — especially in the first year of life.
- How does the human gut change from a totally
germ-free place — in the womb— to one filled with billions of bacteria?
And why does the change happen so differently in different babies?
- It is an amazing thing trying to figure out how we go
from a completely sterile gut to having a microbial ecosystem that will
be with us for the rest of our lives.
- Mostly these bacteria in the digestive system help
the human host. They digest food and kill off harmful bacteria. They
also play a role in defining how much fat a person puts on.
Please click on the line outside the line outside the box
to continue reading about this biological research and also lots of
knowledge as continuation of the left side column.
PVAF, as usual, is publishing today's news story with an
intention TO MAKE
YOUR TOMORROW HAPPIER THAN TODAY....by awakening to the
simple fact that how little we as humanity of today know about ourselves and
our Creator who designs, operates and maintains our bodies for all our
egoistic thinking that:
- I only can do this;
- Without me another cannot exist; and worst of all ego
- I do not believe in a higher power called Creator....
(This article was prepared for publication by
Champaklal Dajibhai Mistry with a prayer
that all humanity will search for the TRUTH about us and our existence
through the study of vED which is the sNskRut language name encompassing all
the sciences which creates this life with its universes, sustains all that
is created and cyclically recycles all that is created through what is
called birth-death cycle....)
|
|
|
Researchers delve into infant gut
by studying what comes out of it
Fourteen babies donate their diapers to study
how bacteria colonize the intestinal
tract
Edmonton Journal:
June 26, 2007: CanWest News Service, Tom s.
Pears
Two U.S. medical institutes have teamed up to explore a
poorly understood material that regulates everything from your immune system
to how you digest food: baby poop. Yes, this is serious science. Fourteen
babies provided raw material for the study, which is trying to solve a
puzzle: How does the human gut change from a totally germ-free place — in
the womb— to one filled with billions of bacteria? And why does the change
happen so differently in different babies?
The medical world knows our DNA from one end to the other, but can’t say the
same about the intestine — especially in the first year of life.
The effects last a lifetime. “It’s an amazing thing trying to figure out how
we go from a completely sterile gut to having a microbial ecosystem that
will be with us for the rest of our lives,” said the study’s senior author,
Dr. Patrick Brown of Stanford University’s faculty of medicine. “What could
be more fundamental than that?”
California’s Stanford and the Howard Hughes Medical Institute in Maryland
joined in the study.
Though newborns have no microbes in the intestine, these arrive within the
first few days. Some are picked up from the mother during birth, others
arrive in food and from the outside world.
There is soon such a thriving community that scientists call the gut “an
ecosystem,” as if it were a jungle or a river.
Soon there are 10 times more bacteria in the gut than there are cells in the
baby’s entire body.
Mostly these bacteria help the human host. They digest food and kill off
harmful bacteria. They also play a role in defining how much fat a person
puts on. And people who take large amounts of antibiotics can upset the
balance in their intestines, as antibiotics kill pathogens and “friendly”
bacteria alike.
|
A year’s worth of samples from the diapers of 14 healthy,
full-term babies showed there are still mysteries in a process every parent
knows all too well. Among them:
- The intestine has close to 400 types of bacteria, but
about half of these have not yet been identified by science.
- The 14 babies picked up very different blends of
bacteria at different times in their first year. But by the end of the
year, they all had a similar mix that’s expected to remain for the long
term. No one knows why the early differences occur.
- Along the way, each individual baby showed huge
swings in which bacteria were present, with certain types becoming
common, but then being replaced by other types.
- There was one pair of non-identical twins in the
study, and they had a very similar group of bacteria all the way through
the year. That may mean the host’s own genes play a role in selecting
how bacteria colonize the gut, the researchers say.
“The fact that the twins were so similar gives us a glimmer of hope that
it’s not a completely chaotic process,” they say in a written summary of
the work.
- The only two babies delivered by caesarean section
had far fewer bacteria of all kinds during their first week. The
researchers think this shows the birth canal is a major source of
microbes for the newborn — though perhaps it doesn’t matter for long.
The study is published today in a science
journal called the Public Library of Science-Biology.
A future phase of the study will compare breast-fed to bottle-fed babies and
will also look at preemies.
|
|
FOR MORE KNOWLEDGE
ON HOW YOU DIGEST LIFE GIVING FOOD
IN YOUR STOMACH AND 32 FT OF ATTACHED TUBE DOWN TO ANUS
PLEASE CONTINUE READING BELOW FROM
WIKIPEDIA, THE FREE ENCYCLOPEDIA SIMILAR TO THIS
FREE-KNOWLEDGE-SHARING PVAF WEB SITE |
Gut flora
From
Wikipedia,
the free encyclopedia
The gut flora are the
microorganisms that normally live in the
digestive tract and can perform a number of useful
functions for their hosts.
The average human body, consisting of about 1013
cells, has about ten times that number of
microorganisms in the gut.[1][2][3][4][5]
Bacteria make up most of the flora in the
colon[5]
and 60% of the mass of
feces.[2]
Somewhere between 300[2]
and 1000 different
species live in the gut,[3]
with most estimates at about 500.[6][4]
However, it is probable that 99% of the bacteria come
from about 30 or 40 species.[7]
Fungi also make up a part of the gut flora, but
little is known about their activities.
Research suggests that the relationship between gut
flora and humans is not merely
commensal (a non-harmful coexistence), but rather is
a
mutualistic,
symbiotic relationship.[3]
Though people can survive with no gut flora,[4]
the microorganisms perform a host of useful functions,
such as
fermenting unused energy substrates, training the
immune system, preventing growth of harmful species,[2]
regulating the development of the gut, producing
vitamins for the host (such as
biotin and
vitamin K), and producing hormones to direct the
host to store fats. However, in certain conditions, some
species are thought to be capable of causing
disease by causing
infection or increasing
cancer risk for the host.[2][5]
[edit]
Localization
The colon has the greatest numbers of bacteria and
the most different species, and the activity of these
bacteria make the colon the most
metabolically active
organ in the body.[6]
Most of the bacteria in the small intestine are
Gram-positive, while those in the colon are mostly
Gram-negative.[8]
The first part of the colon is mostly responsible for
fermenting
carbohydrates,[7][6][2]
while the latter part mostly breaks down
proteins and
amino acids.[6][2]
Bacterial growth is rapid in the
cecum and
ascending colon, which has a low
pH,
and slow in the descending colon, which has an almost
neutral pH.[2]
The body maintains the proper balance and locations of
species by altering pH, the activity of the immune
system, and
peristalsis.[5]
Over 99% of the bacteria in the gut are
anaerobes,[7][2][5][3][9]
but in the
cecum
aerobic bacteria reach high densities.[2]
Not all the species in the gut have been identified[2][3]
because some cannot be cultured,[7][3][10]
so DNA isolation and identification is difficult.[11]
Populations of species vary widely among different
individuals but stay fairly constant within an
individual over time.[2]
Most bacteria come from the genera
Bacteroides,
Clostridium,
Fusobacterium,[7][2][9]
Eubacterium,
Ruminococcus,
Peptococcus,
Peptostreptococcus, and
Bifidobacterium.[2][7]
Other genera such as
Escherichia and
Lactobacillus are present to a lesser extent.[2]
Species from the genus Bacteroides alone
constitute about 30% of all bacteria in the gut,
suggesting that that genus is especially important in
the functioning of the host.[3]
The currently known genera of
fungi of the gut flora include
Candida,
Saccharomyces,
Aspergillus, and
Penicillium.
[edit]
Acquisition of gut flora in
human infants
The
gastrointestinal tract of a normal
fetus is sterile. During birth and rapidly
thereafter, bacteria from the mother and the surrounding
environment colonize the infant gut. Immediately after
vaginal delivery, babies have bacterial strains in the
upper gastrointestinal tract derived from the mothers’
feces.[12]
Infants born by
caesarean section may also be exposed to their
mothers’ microflora, but the main exposure is from the
surroundings.[13]
After birth, environmental, oral and
cutaneous bacteria are readily transferred from the
mother to the infant through
suckling, kissing, and caressing. All infants are
initially colonized by large numbers of
E. coli and
streptococci. Within a few days, bacterial numbers
reach 108 – 1010 /g
feces.[13][14]
During the first week of life, these bacteria create a
reducing environment favorable for the subsequent
bacterial
succession of strict
anaerobic species mainly belonging to the genera
Bifidobacterium,
Bacteroides,
Clostridium, and
Ruminococcus.[15]Breast-fed
babies become dominated by
bifidobacteria, possibly due to the contents of
bifidobacterial growth factors in breast milk.[16]
In contrast, the microflora of
formula-fed infants is more diverse with high
numbers of
Enterobacteriaceae,
enterococci,
bifidobacteria,
Bacteroides, and
clostridia.[17][18]
After the introduction of solid food and
weaning, the microflora of breast-fed infants
becomes similar to that of formula-fed infants. By the
second year of life the fecal microflora resembles that
of adults.
[edit]
Functions
Bacteria in the gut fulfills a host of useful
functions for humans, including digestion of unutilized
energy substrates;[19]
stimulating cell growth; repressing the growth of
harmful microorganisms; training the immune system to
respond only to
pathogens; and defending against some diseases.[2][3][20]
[edit]
Carbohydrate fermentation and
absorption
Without gut flora, the human body would be unable to
utilize some of the undigested
carbohydrates it consumes, because some types of gut
flora have
enzymes that human cells lack for breaking down
certain
polysaccharides.[3]
Rodents raised in a sterile environment and lacking in
gut flora need to eat 30% more
calories just to remain the same weight as their
normal counterparts.[3]
Carbohydrates that humans cannot
digest without bacterial help include certain
starches;
fiber;
oligosaccharides and
sugars that the body failed to digest and absorb[6][2][7]
like
lactose and sugar
alcohols,
mucus produced by the gut, and proteins.[6]
Bacteria turn carbohydrates they ferment into
short chain fatty acids, or SCFAs.[6][5][7]
These materials can be used by host cells, providing a
major source of useful energy and nutrients for humans.[6]
They increase the gut's absorption of water, reduce
counts of damaging bacteria, increase growth of human
gut cells,[5]
and are also used for the growth of indigenous bacteria.[2]
The SCFAs are produced by a form of fermentation called
saccharolytic fermentation[6]
and include
acetic acid,
propionic acid, and
butyric acid.[6][5][7]
Gases and
organic acids like
lactic acid are also produced by saccahrolytic
fermentation.[7]
Acetic acid is used by
muscle, propionic acid helps the
liver produce
ATP, and butyric acid provides energy to gut cells
and may prevent
cancer.[6]
Another, less favorable type of fermentation,
proteolytic fermentation, breaks down proteins like
enzymes, dead host and bacterial cells, and
collagen and
elastin found in food, and can produce toxins and
carcinogens in addition to SCFAs. Thus a diet lower
in protein lowers exposure to toxins.[2][5]
Evidence also suggests that bacteria enhance the
absorption and storage of
lipids.[3]
Bacteria also produce and help the body absorb needed
vitamins like vitamin K. In addition, the SCFAs they
produce help the body absorb nutrients such as
calcium,
magnesium, and
iron.[2]
[edit]
Trophic effects
Another benefit of SCFAs is that they increase growth
of intestinal
epithelial cells and control their proliferation and
differentiation.[2]
They may also cause
lymphoid tissue near the gut to grow. Bacterial
cells also alter intestinal growth by changing the
expression of
cell surface proteins such as
sodium/glucose transporters.[3]
In addition, changes they make to cells may prevent
injury to the gut
mucosa from occurring.[20]
[edit]
Repression of pathogenic
microbial growth

C. difficile colonies on a blood
agar plate. The overgrowth of C.
difficile in the gut can be harmful to
the host.
Another important role of helpful gut flora is that
they prevent species that would harm the host from
colonizing the gut, an activity termed the "barrier
effect".
Yeasts and harmful bacterial species such as
Clostridium difficile (the overgrowth of which
can cause
pseudomembranous colitis) are unable to grow too
much due to competition from helpful gut flora species,
thus animals without gut flora are
infected very easily. The barrier effect protects
humans from both invading species and species normally
present in the gut at low numbers, whose growth is
usually inhibited by the gut flora.[2]
Helpful bacteria prevent the growth of pathogenic
species by competing for nutrition and
attachment sites to the
epithelium of the colon. Symbiotic bacteria are more
at home in this ecological niche and are thus more
successful in the competition. The indigenous bacteria
send chemical signals to the host about the amount of
nutrients they need, and the host provides only that
much, so harmful bacteria are starved out. Indigenous
gut flora also produce
bacteriocins, substances which kill harmful microbes
and the levels of which can be regulated by enzymes
produced by the host.[2]
The process of fermentation, since it produces
fatty acids, also serves to lower the pH in the
colon, preventing the proliferation of harmful species
of bacteria and facilitating that of helpful species.
The pH may also enhance the excretion of carcinogens.[6]
[edit]
Immunity
Gut flora have a continuous and dynamic effect on the
host's gut and systemic immune systems. The bacteria are
key in promoting the early development of the gut's
mucosal immune system both in terms of its physical
components and function and continue to play a role
later in life in its operation. The bacteria stimulate
the lymphoid tissue associated with the gut mucosa to
produce antibodies to pathogens. The immune system
recognizes and fights harmful bacteria, but leaves the
helpful species alone, a tolerance developed in infancy.[2][10][4][5]
As soon as an infant is born, bacteria begin
colonizing its digestive tract. The first bacteria to
settle in are able to affect the
immune response, making it more favorable to their
own survival and less so to competing species; thus the
first bacteria to colonize the gut are important in
determining the person's lifelong gut flora makeup.
However, there is a shift at the time of
weaning from predominantly
facultative aerobic species such as
Streptococci and
Escherichia coli to mostly
obligate anaerobic species.[2][3]
Recent findings have shown that gut bacteria play a
role in the expression of
Toll-like receptors (TLRs) in the intestines,
molecules that help the host repair damage due to
injury. TLRs cause parts of the immune system to repair
injury caused for example by
radiation.[3][20]
Bacteria can influence the phenomenon known as
oral tolerance, in which the immune system is less
sensitive to an
antigen (including those produced by gut bacteria)
once it has been ingested. This tolerance, mediated in
part by the gastrointestinal immune system and in part
by the liver, can reduce an overreactive immune response
like those found in
allergies and
auto-immune disease.[21]
Some species of gut flora, such as some of those in
the Bacteroides genus, are able to change their
surface receptors to mimic those of host cells in order
to evade immune response. Bacteria with neutral and
harmful effects on the host can also use these types of
strategies. The host immune system has also adapted to
this activity, preventing overgrowth of harmful species.[2][4]
[edit]
Preventing allergy
Bacteria are also implicated in preventing
allergies,[1]
an overreaction of the immune system to non-harmful
antigens. Studies on the gut flora of infants and
young children have shown that those who have or later
develop allergies have different compositions of gut
flora from those without allergies, with higher chances
of having the harmful species C difficile and
S aureus and lower prevalence of Bacteroides
and Bifidobacteria.[1]
One explanation is that since helpful gut flora
stimulate the immune system and "train" it to respond
properly to antigens, a lack of these bacteria in early
life leads to an inadequately trained immune system
which overreacts to antigens.[1]
On the other hand, the differences in flora could be a
result, not a cause, of the allergies.[1]
[edit]
Preventing inflammatory bowel
disease
Another indicator that bacteria help train the immune
system is the
epidemiology of
Inflammatory Bowel Disease, or IBD, such as
Crohn's Disease (CD). Some authors suggest that
SCFAs prevent IBD. In addition, some forms of bacteria
can prevent
inflammation.[22]
The incidence and prevalence of IBD is high in
industrialized countries with a high
standard of living and low in
less economically developed countries, having
increased in developed countries throughout the
twentieth century. The disease is also linked to good
hygiene in youth; lack of breastfeeding; and consumption
of large amounts of sucrose and animal fat.[22]
Its incidence is inversely linked with poor sanitation
during the first years of life and consumption of
fruits, vegetables, and unprocessed foods.[22]
Also, the use of antibiotics, which kill native gut
flora and harmful infectious pathogens alike, especially
during childhood, is associated with inflammatory bowel
disease.[19]
On the other hand, using
probiotics, bacteria consumed as part of the diet
that impart health benefits (aside from just
nutrition), helps treat IBD.
[edit]
Alterations in balance
[edit]
Effects of antibiotic use
Altering the numbers of gut bacteria, for example by
taking
broad-spectrum antibiotics, may affect the host's
health and ability to digest food.[23]
People may take the drugs to cure bacterial illnesses or
may unintentionally consume significant amounts of
antibiotics by eating the meat of animals to which
they were fed.[23]
Antibiotics can cause
antibiotic-associated diarrhea (AAD) by irritating
the
bowel directly, changing the levels of gut flora, or
allowing
pathogenic bacteria to grow.[7]
Another harmful effect of antibiotics is the increase in
numbers of
antibiotic-resistant bacteria found after their use,
which, when they invade the host, cause illnesses that
are difficult to treat with antibiotics.[23]
Changing the numbers and species of gut flora can
reduce the body's ability to ferment carbohydrates and
metabolize
bile acids and may cause diarrhea. Carbohydrates
that are not broken down may absorb too much water and
cause runny stools, or lack of SCFAs produced by gut
flora could cause the diarrhea.[7]
A reduction in levels of native bacterial species
also disrupts their ability to inhibit the growth of
harmful species such as C. difficile and
Salmonella kedougou, and these species can get
out of hand, though their overgrowth may be incidental
and not be the true cause of diarrhea.[7][23][2]
Gut flora composition also changes in severe
illnesses, due not only to antibiotic use but also to
such factors as
ischemia of the gut, failure to eat, and
immune compromise. Negative effects from this have
led to interest in
selective digestive tract decontamination (SDD), a
treatment to kill only pathogenic bacteria and allow the
reestablishment of healthy ones.[24]
[edit]
Probiotics & Prebiotics
Since the lack of gut flora can have such harmful
health effects, the use of
probiotics has anti-inflammatory
effects in the gut and may be useful for improving
health.
Prebiotics are dietary components that can help
foster the growth of microorganisms in the gut, which
may lead to better health.[22]
[edit]
Role in disease
Bacteria in the digestive tract have pathogenic
properties in addition to their health-inducing ones:
they can produce
toxins and
carcinogens[5]
and have been implicated in such conditions as
multisystem organ failure,
sepsis,
colon cancer, and IBD.[2]
A major factor in health is the balance of bacterial
numbers; if the numbers grow too high or low, it will
result in harm to the host. The host has
enzymes to regulate this balance.[5]
[edit]
Cancer
Some
genera of bacteria, such as Bacteroides and
Clostridium, have been associated with an
increase in
tumor growth rate, while other genera like
Lactobacillus and Bifidobacteria are known to
prevent tumor formation.[2]
[edit]
Translocation
Helpful bacteria can be very harmful to the host if
they get outside of the intestinal tract.[3][5][9]
Translocation, which occurs when bacteria leave the
gut through its
mucosal lining, the border between the
lumen of the gut and the inside of the body,[4][25]
can occur in a number of different diseases.[9][22]
It can be caused by too much growth of bacteria in the
small intestine, reduced immunity of the human, or
increased gut lining permeability.[22]
The gut can become more permeable in diseases like
cirrhosis, which is damaging due in part to the
activity of gut flora.[26]
If the gut is perforated, bacteria can invade the
body, causing a potentially fatal infection. Aerobic
bacteria can make infection by anaerobes worse by using
up all available oxygen and creating an environment
favorable to anaerobes.[9]
[edit]
Inflammatory bowel disease
Some suspect that IBD is due to a reduction in immune
tolerance and subsequent overreaction of the host's
immune system to harmful or non-harmful bacteria. IBD
may be caused by all of the gut flora together or some
specific types.[27][19]
It has been noted that though
Ulcerative Colitis and
Crohn's disease (two types of IBD) probably have
genetic components, they are not inherited in a
Mendelian fashion and are thus probably due to a
complex set of factors rather than solely to a
gene.[27]
Though neither bacterial colonization nor
genetics is sufficient to cause the disease,
bacteria probably play a role in these disorders.[27]
Some suspect that inflammation in IBD is due to
increased permeability of the inner lining of the colon,
which may allow bacteria to invade the tissues and cause
an immune reaction that leads prolonged inflammation.[4][25]
Abnormal
tight junctions, which are supposed to prevent
permeability, have been found in cells of patients with
IBD.[25]
Because of the potentially harmful role of these
bacteria, antibiotics are frequently prescribed to treat
Crohn’s disease.[20]
However, inflammation could occur first and cause the
increased intestinal permeability found in diseases such
as Crohn's, so the causative role of bacteria is not
clear.[25]
[edit]
Colitis
It has been suggested that commensal bacteria are
responsible for the development of
colitis, since mice raised in a
sterile environment do not get the disease.[28]
However, while some bacterial strains such as C.
difficile[22]
and even normal gut bacteria cause colitis,[28]
others prevent the disease in mice.[22]
[edit]
Sources and notes
- ^
a
b
c
d
e Björkstén B, Sepp E, Julge K,
Voor T, and Mikelsaar M. 2001.
Allergy development and the intestinal microflora
during the first year of life. Journal of
Allergy and Clinical Immunology, Volume 108,
Issue 4, Pages 516-520. Accessed
January 9,
2007
-
^
a
b
c
d
e
f
g
h
i
j
k
l
m
n
o
p
q
r
s
t
u
v
w
x
y
z
aa
ab
ac Guarner F and
Malagelada JR. 2003b.
Gut flora in health and disease. The Lancet,
Volume 361, Issue 9356, 8 February 2003, Pages
512-519. Accessed
January 7,
2007
- ^
a
b
c
d
e
f
g
h
i
j
k
l
m
n
o
Sears CL. 2005.
A dynamic partnership: Celebrating our gut flora.
Anaerobe, Volume 11, Issue 5, Pages 247-251.
Accessed
January 7,
2007
- ^
a
b
c
d
e
f
g
Steinhoff U. 2005.
Who controls the crowd? New findings and old
questions about the intestinal microflora.
Immunology Letters, Volume 99, Issue 1, 15 June
, Pages 12-16. Accessed
January 9,
2007
- ^
a
b
c
d
e
f
g
h
i
j
k
l
m University of Glasgow.
2005.
The normal gut flora. Available through web
archive. Accessed
December 26,
2006
- ^
a
b
c
d
e
f
g
h
i
j
k
l
Gibson RG. 2004. Fibre and effects on probiotics
(the prebiotic concept). Clinical Nutrition
Supplements, Volume 1, Issue 2, Pages 25-31.
-
^
a
b
c
d
e
f
g
h
i
j
k
l
m Beaugerie L and Petit
JC. 2004.
Microbial-gut interactions in health and disease.
Antibiotic-associated diarrhoea. Best
Practice & Research Clinical Gastroenterology,
Volume 18, Issue 2, Pages 337-352. Accessed
January 9,
2007
-
^ Riordan
SM, McIver CJ, Wakefield D, Duncombe VM, Thomas MC,
and Bolin TD. 2001.
Small intestinal mucosal immunity and morphometry in
luminal overgrowth of indigenous gut flora.
The American Journal of Gastroenterology, Volume
96, Issue 2, Pages 494-500. Accessed
January 9,
2007
- ^
a
b
c
d
e
Vedantam G and Hecht DW. 2003.
Antibiotics and anaerobes of gut origin.
Current Opinion in Microbiology, Volume 6, Issue
5, Pages 457-461. Accessed
January 9,
2007
- ^
a
b
Shanahan F. 2002.
The host–microbe interface within the gut.
Best Practice & Research Clinical Gastroenterology,
Volume 16, Issue 6, Pages 915-931. Accessed
January 7,
2007
-
^
Nordgård L, Traavik T, and Nielsen KM. 2005.
Nucleic Acid Isolation from Ecological
Samples—Vertebrate Gut Flora. Methods in
Enzymology, Volume 395, Pages 38-48. Accessed
January 9,
2007
-
^
Bettelheim KA, Breadon A, Faiers MC, O'Farrell SM,
Shooter RA. 1974. The origin of O serotypes of
Escherichia coli in babies after normal delivery. J
Hyg (Lond).72:67-70.[
- ^
a
b
Schwiertz A, Gruhl B, Lobnitz M, Michel P, Radke M,
Blaut M. 2003. Development of the intestinal
bacterial composition in hospitalized preterm
infants in comparison with breast-fed, full-term
infants. Pediatr Res. 54:393-9.
-
^ Mackie RI,
Sghir A, Gaskins HR. 1999. Developmental microbial
ecology of the neonatal gastrointestinal tract. Am J
Clin Nutr. 69:1035S-1045S.
-
^ Favier CF,
Vaughan EE, De Vos WM, Akkermans AD. 2002. Molecular
monitoring of succession of bacterial communities in
human neonates. Appl Environ Microbiol. 68:219-26.
-
^ Coppa GV,
Bruni S, Morelli L, Soldi S, Gabrielli O. 2004. The
first prebiotics in humans: human milk
oligosaccharides. J Clin Gastroenterol. 38(6
Suppl):S80-3.
-
^ Harmsen
HJ, Wildeboer-Veloo AC, Raangs GC, Wagendorp AA,
Klijn N, Bindels JG, Welling GW. 2000. Analysis of
intestinal flora development in breast-fed and
formula-fed infants by using molecular
identification and detection methods. J Pediatr
Gastroenterol Nutr. 30:61-7.
-
^ Fanaro S,
Chierici R, Guerrini P, Vigi V. 2003. Intestinal
microflora in early infancy: composition and
development. Acta Paediatr Suppl. 91(441):48-55.
- ^
a
b
c
Wynne AG, McCartney AL, Brostoff J, Hudspith BN,
Glenn GR and Gibson G. 2004.
An in vitro assessment of the effects of
broad-spectrum antibiotics on the human gut
microflora and concomitant isolation of a
Lactobacillus plantarum with anti-Candida
activities. Anaerobe, Volume 10, Issue 3,
Pages 165-169. Accessed
January 9,
2007
- ^
a
b
c
d
Keeley J. 2004.
Good bacteria trigger proteins to protect the gut.
Howard Hughes Medical Institute. EurekAlert.
Accessed
January 9,
2007
-
^ Jewell AP.
2005.
Is the liver an important site for the development
of immune tolerance to tumours? Medical
Hypotheses, Volume 64, Issue 4, Pages 751-754.
Accessed
January 9,
2007
-
^
a
b
c
d
e
f
g
h Guarner F and
Malagelada JR. 2003a.
Role of bacteria in experimental colitis. ‘’Best
Practice & Research Clinical Gastroenterology’’,
Volume 17, Issue 5, October 2003, Pages 793-804.
Accessed
January 7,
2007
- ^
a
b
c
d
Carman RJ, Simon MA, Fernández H, Miller MA, and
Bartholomew MJ. 2004.
Ciprofloxacin at low levels disrupts colonization
resistance of human fecal microflora growing in
chemostats. Regulatory Toxicology and
Pharmacology, Volume 40, Issue 3, December,
Pages 319-326. Accessed
January 7,
2007
-
^ Knight DJW
and Girling KJ. 2003.
Gut flora in health and disease. The Lancet,
Volume 361, Issue 9371, Page 1831. Accessed
January 7,
2007
- ^
a
b
c
d
Suenaert P, Bulteel V, Lemmens L, Noman M, Geypens
B, Assche GV, Geboes K, Ceuppens JL and Rutgeert P.
2002.
Anti-tumor necrosis factor treatment restores the
gut barrier in Crohn’s disease. The American
Journal of Gastroenterology, Volume 97, Issue 8,
Pages 2000-2004. Accessed
January 7,
2007
-
^
Garcia-Tsao G and Wiest R. 2004.
Gut microflora in the pathogenesis of the
complications of cirrhosis. Best Practice &
Research Clinical Gastroenterology, Volume 18,
Issue 2, Pages 353-372. Accessed
January 9,
2007
- ^
a
b
c
Hugot JP. 2004.
Inflammatory bowel disease: a complex group of
genetic disorders. Best Practice & Research
Clinical Gastroenterology, Volume 18, Issue 3,
Pages 451-462. Accessed
January 9,
2007
- ^
a
b
Veltkamp C, Tonkonogy SL, De Jong YP, Albright C,
Grenther WB, Balish E, Terhorst C, and Sartor RB.
2001.
Continuous stimulation by normal luminal bacteria is
essential for the development and perpetuation of
colitis in Tg(epsilon26) mice.
Gastroenterology, Volume 120, Issue 4, Pages
900-913. Accessed
January 7,
2007
|
|
There are 0 additional comments.
Send your news items
to be posted to news@prajapati-samaj.ca.
|